|
The Strabismus Research Foundation is a 501(c)(3) non-profit operating foundation (EIN 46-1989857) devoted to translational research in ocular motility. Eidactics ("eye-DAK-tics") is a California company (EIN 20-4569747) conducting pure and applied oculomotor research.
|
|
A Light Has Gone Out
|
|
Alan Scott died peacefully on 2021-12-16, with family, friends and colleagues at his bedside and on Internet. "Don't mourn me", he asked, "I've had close to 90 years of a good life". His life was indeed good for everyone who was part of it. Alan was bold, brilliant and kind, always intending to do the most good and the least harm.
We cope with loss by internalizing something of what the world no longer provides. Alan was my colleague, ally and friend for 40 years, lastly working at the independent lab we built. I've now to close that lab and retire from research, and find myself regarding those changes with the amused pragmatism Alan might have.
|
|

|
Alan B Scott, MD
- Director & Senior Scientist at The Strabismus Research Foundation (SRF), and Senior Scientist at Eidactics (2013-2021).
- Senior Scientist at The Smith-Kettlewell Eye Research Institute (SKERI; 1959-2016).
|
|

|
Joel M Miller, PhD
- Director & Senior Scientist at Eidactics, and Director of Research at The Strabismus Research Foundation (SRF).
- Senior Scientist at The Smith-Kettlewell Eye Research Institute (SKERI; 1982-2013).
|
|
|
|
STRABOS 2025 Lectures
|
- EOM Pulleys and Compartments - Sense and Nonsense PDF MP4
- Biomechanical Analysis of Strabismus Strengths and Limitations PDF MP4
- Injection vs Incisional Treatment of Strabismus PDF MP4
|
|
Ongoing Project
|
|
|
Immunohistochemical & Biomechanical Effects of Bupivacaine Injection on Rabbit EOM
Prior to closing our lab at the end of 2021 we completed several lines of work on bupivacaine injection treatment (see below): delineating the advantages of pharmacologic injection compared to incisional surgery, as well as its limitations; developing bupivacaine dosage guidelines; injecting over 200 patients with outcomes comparable to surgery; documenting the time course of corrections and muscle hypertrophy (Miller et al, 2013; Debert et al, 2016); developing a combined EMG–stimulation device for targeting injections in both awake and anesthetized patients (see srfsf.org or eidactics.com). Nevertheless, many basic questions remain about the effects of bupivacaine injection on overall muscle contractility, muscle stiffness, distribution of muscle fiber types and sizes, and type and amount of intramuscular connective tissue. More remains to be done to characterize patients most suitable for injection treatment.
The SRF Board of Directors is therefore pleased to announce funding of a project at UCSD's Shiley Eye Institute, "Immunohistochemical and Biomechanical Effects of Bupivacaine Injection on Rabbit Extraocular Muscle”, PI Jolene Rudell MD, PhD at $377,789 for the first year, with optional 2nd year. We've also donated equipment used in our closely related projects, including a Leica DM6000B microscope and an Aurora muscle measurement system, to enable Dr Rudell to continue and extend this research, which we believe to be critical to advancing pharmacologic injection treatment of strabismus.
|
|
Completed Projects
|
 |
Pharmacologic Injection Treatment of Strabismus
Strabismus, misalignment of the eyes, is mostly treated surgically by compensatory impairment of healthy muscles, rather than by correcting the underlying disorder. Incisional surgery is costly, results in scarring that makes frequently-needed followup surgery difficult, and requires general anesthesia that may be problematic in some populations (smarttots.org). We have long been interested in pharmacologic injection treatments to supplement or replace conventional surgery:
-
Debert I, Miller JM (2015). Injection Treatment of Strabismus. Eidactics. (PDF)
Oculinum® (now called Botox®) was originally developed to relax and lengthen "tight" eye muscles (Scott 1980). It was the first successful pharmacologic injection treatment for strabismus, and the first therapeutic application of botulinum toxin. So dauntingly counterintuitive was the notion of injecting this most toxic substance, without visual guidance, alongside the healthy eye of an alert patient, that its safe and efficacious development, and the many and varied applications that followed, make a uniquely fascinating story of medical discovery:
- Debert I, Miller JM (2015) History of Botulinum Toxin Therapy. Eidactics. (PDF, On Wikipedia)
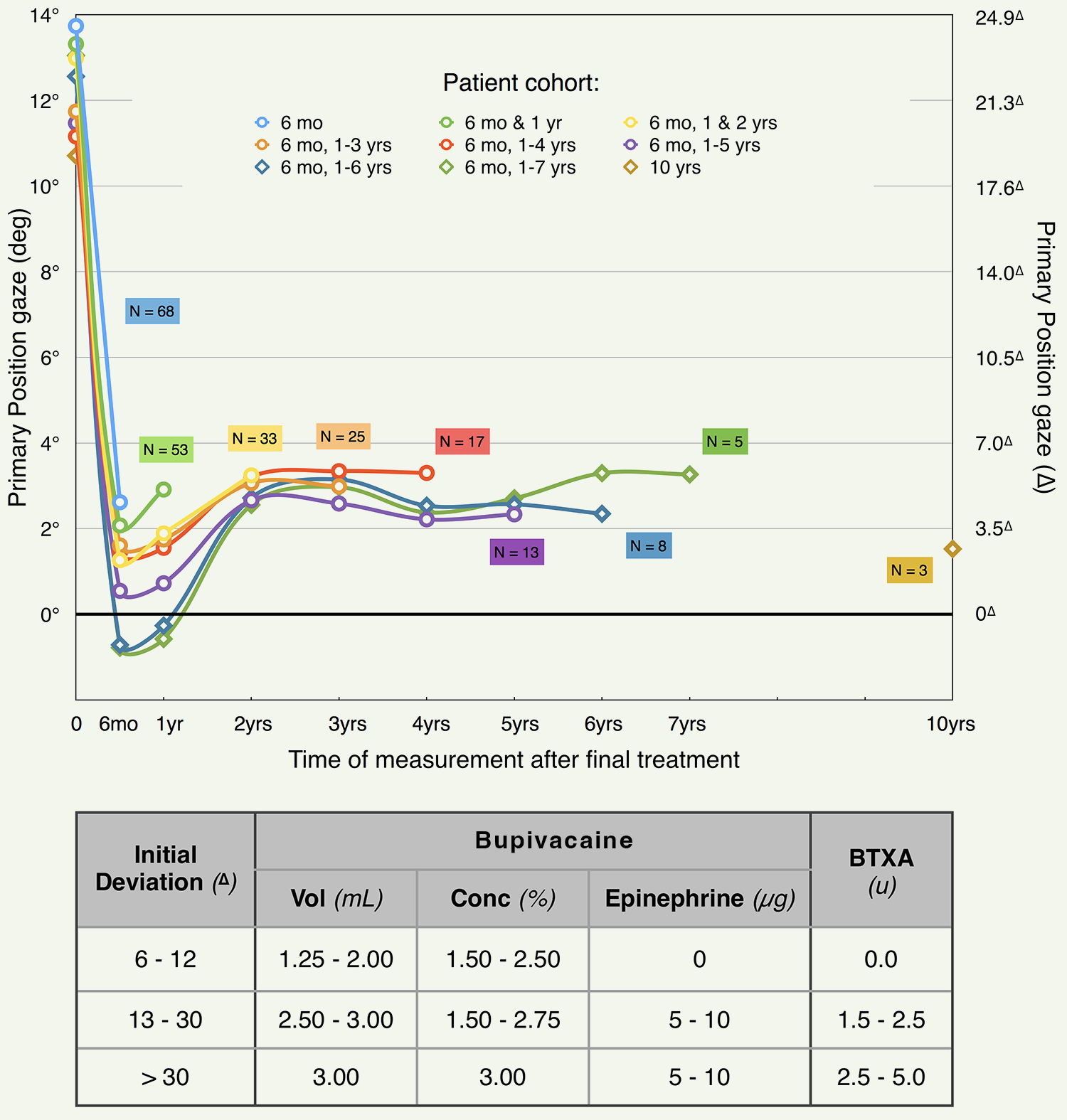
We then worked on the problem of strengthening and shortening "weak" muscles. Bupivacaine (BUP) is a selective myotoxin with effects analogous to mechanical overloading – myofiber damage followed by hypertrophy – and we have been developing BUP injection as a practical method for correcting eye misalignments. Bupivacaine dissociates sarcomeres (the muscle's contractile elements), triggering satellite cells (a kind of stem cell) to rebuild the damaged fibers, stronger, stiffer, and at reduced length. Almost 200 volunteer strabismus patients have received BUP injection treatments, most also with botulinum toxin in the antagonist muscle to prevent stretching while the BUP-injected muscle rebuilds:
-
Miller JM, Scott AB, Danh KK, Strasser D, Sane M (2013).
Bupivacaine injection remodels extraocular muscles & corrects comitant strabismus.
Ophthalmology, vol 120, num 12, December. (Authors' Cut PDF Publisher's site)
-
Debert I, Miller JM, Danh KK, Scott AB (2016).
Pharmacologic Injection Treatment of Comitant Strabismus.
Journal of AAPOS, vol 20, pgs 106-111. (Authors' Cut PDF; Publisher's site)
-
Cunha TM, Miller JM, Scott AB (2018).
Injection of Bupivacaine & Botulinum Type A Toxin to Treat Strabismus.
Transactions of ISA. (Manuscript PDF)
Injection treatment for horizontal strabismus achieves stable corrections which we've tracked up to 10 yrs (each curve in the associated graph shows alignment data for a cohort of patients who all returned for the same followup measurements). Dosage guidelines are shown in the table.
Having demonstrated the clinical effectiveness of BUP treatment in comitant adult strabismus, we developed injection techniques suitable for children (see below). BUP injection may also have clinical applications in other small muscles.
|
|
|
|
Accurate Injection of Eye Muscles in Children (Knights Templar Eye Foundation • Taliva D Martin, MD & Alan B Scott, MD)
Early treatment of infantile strabismus facilitates normal development of stereopsis (depth perception from binocular vision), prevents amblyopia (suppression of vision in one eye), and improves cosmesis. But surgical correction in young children is problematic: [1] frequently necessary follow-up surgery is made more difficult by scarring from the initial surgery; it would be better if non-surgical treatment were used, at least initially, and [2] strabismus surgery requires prolonged general anesthesia, which may cause cognitive deficits in a developing brain (eg, Rappaport et al 2015).
Botulinum toxin A (BTXA) injection treatment of Extraocular muscles (EOMs) is an effective and widely-accepted alternative to conventional surgical treatment of esotropia. Because EOMs lie deep in the orbit, a technique is needed to accurately place the injection needle within the target muscle. In awake, cooperative adults, electromyography (EMG) signals are recorded from the tip of the injection needle, which is advanced until the relationship of the EMG signal to the patient’s voluntary eye movement indicates desired placement.
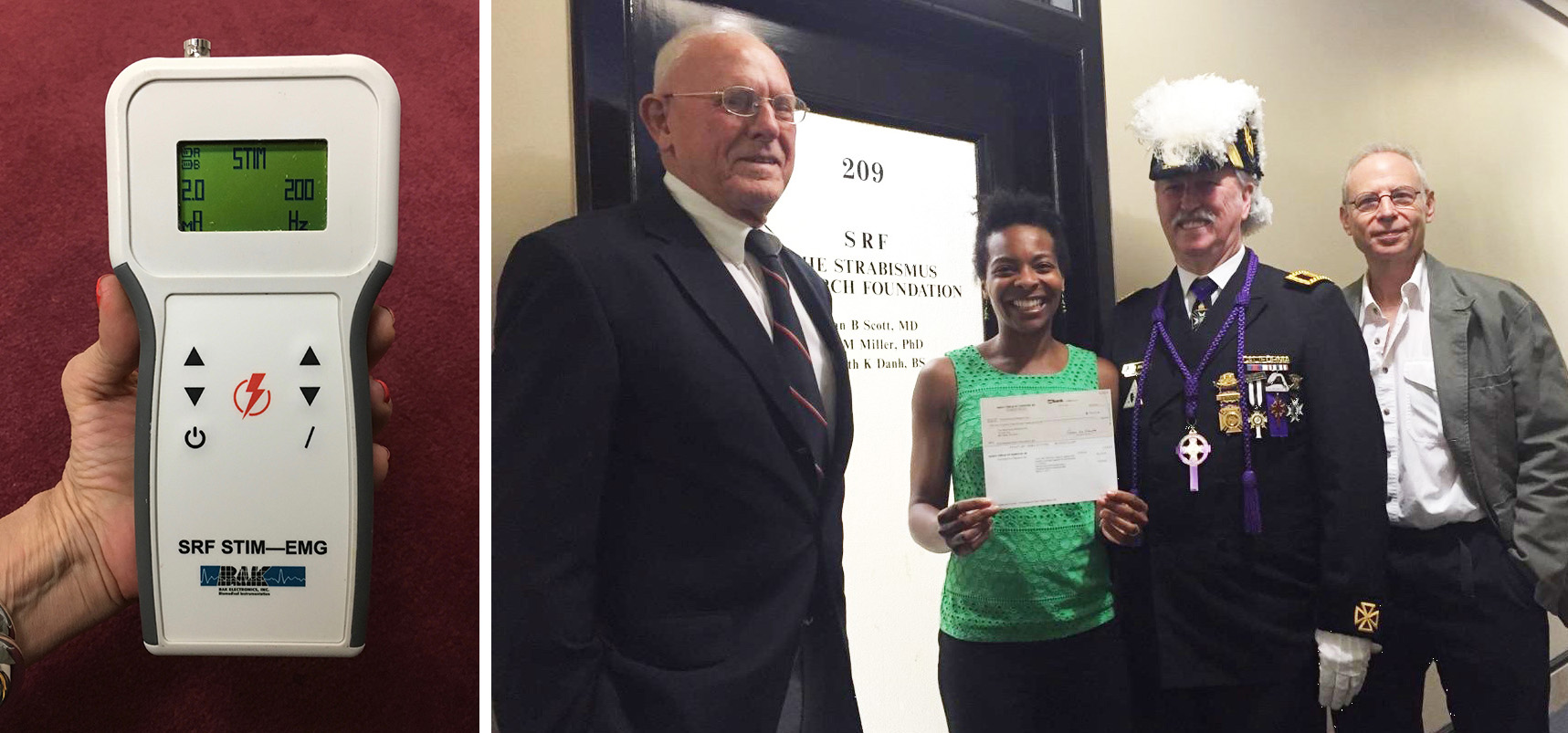
But most strabismus patients are children, who must be briefly anesthetized to accept injection treatment, and anesthetized muscles show little or no movement-related electrical activity. Injection treatment in children is therefore currently performed without EMG guidance, and so, cannot target the deeper neuromuscular junctions, resulting in reduced treatment efficacy and unwanted effects on neighboring muscles. Although no useful EMG signal can be recorded, an anesthetized muscle can be readily stimulated. We have determined from animal studies (funded by The Pacific Vision Foundation) that brief trains of 0.5-5.0 mA, 1 ms square-wave pulses at ~200 Hz produce eye movements characteristic of optimal needle placement. With the support of the Knights Templar Eye Foundation, we developed a suitable stimulating device, and have proposed to evaluate its effectiveness on young strabismus patients. Stimulation-guided injection is expected to be similarly useful in extending to children other pharmacologic injection treatments now under development.
We thank the Knights Templar Eye Foundation for supporting this clinically significant work in its early stages. In the photo, Bud Ramsey, Past Grand Commander, tours SRF's labs and presents the grant check to Drs Martin & Scott.
|
|
|
|
Activating the Levator to Elevate the Eyelid
Blepharospasm sufferers may be functionally blind despite having normal eyes because of spasms in surrounding facial muscles and eyelid apraxia, inability to raise the eyelids or keep them raised. It is a disorder of central control, possibly related to abnormal function of the basal ganglia, but its cause is unknown. The disorder typically affects otherwise healthy adults age 40-60, progresses for a few months and then remains stable for decades. Muscles and nerves are normal, and most patients have periods of normal function – dark rooms, looking downward, even swimming under water are situations they say are helpful.
Botulinum toxin injection can relieve the spasms, but eyelid apraxia often remains. Surgical lid elevation and botulinum toxin injection of the pretarsal orbicularis of the upper lid can be helpful, but static repositioning makes normal eye blinking and lid closure problematic. Functional electrical stimulation (FES) of the muscle that raises the eyelid (the levator palpebrae superioris or LPS), could provide functionally blind patients with useful vision. Programmable, coordinated, binocular FES would be far superior to surgery, both functionally and cosmetically.
|
|

|
Motor Unit Diversity in Horizontal Eye Movement Control (NIH/NEI
The Missing Force Paradox (see below) implies that some motoneurons don't much contribute to oculorotary force. Microanatomy also suggests that some motor units don't directly rotate the eye (eg, Oh, 2001), and that nonlinear interactions among muscle fibers (eg, Goldberg et al, 1997) may be the norm. We are therefore keen to characterize the participation of individual motor units in different types of eye movement.
Extraocular muscle (EOM) fibers are of several distinct types (egs, Spencer and Porter, 1988; McLoon etal 2011), and a given motoneuron (MN) innervates fibers of only one type, implying that there are different types of motor units (MUs; each a motor neuron and its muscle fibers). Nevertheless, classical studies of oculomotor physiology consider all MNs to be fundamentally the same, differing only quantitatively. Individual MUs have been studied only crudely, using electrical stimulation in anesthetized animals.
To study MUs in alert behaving NHPs we recorded MN activity with extracellular electrodes, and extraocular muscle force with muscle force transducers (MFTs). During steady fixation with low motoneuron firing rates, we used spike-triggered averaging of MFT signals (STA-MFT) to extract single muscle twitches, thereby characterizing individual MUs. (It would then be possible to measure participation of a characterized MU during eye movements involving high or rapidly-varying MN firing rates).
-
Gamlin PD, Miller JM (2012). Extraocular muscle motor units characterized by spike-triggered averaging in alert monkey. Journal of Neuroscience Methods, vol 204, pgs 159-167. (Authors' Cut PDF; Publisher's site)
|
|
|
|
Missing Force Paradox
For a given eye position, firing rates of abducens neurons (ABNs) generally (Mays et al 1984), and lateral rectus motoneurons (MNs) in particular (Gamlin et al 1989a), are higher in converged gaze than when convergence is relaxed, whereas lateral rectus (LR) and medial rectus (MR) muscle forces are slightly lower (Miller et al 2002). Here, we confirm this finding for ABNs, report a similarly paradoxical finding for neurons in the MR region of the oculomotor nucleus (MR MNs), and for the first time simultaneously confirm the opposing sides of the paradox by recording physiological LR and MR forces.
Consistent with earlier findings, we found in 44 ABNs that the slope of the rate-position relationship for symmetric vergence (kv) was lower than that for conjugate movement (kc) at distance, ie, mean kv/kc = 0.50, which implies stronger LR innervation in convergence. We also found in 39 MR MNs that mean kv/kc = 1.53, implying stronger MR innervation in convergence as well.
Despite there being stronger innervation in convergence at a given eye position we found, confirming previous measurements, that both LR and MR muscle forces were slightly lower in convergence, -0.40 and -0.20 g, respectively.
This implies that the relationship of ensemble MN activity to total oculorotary muscle force is different in converged gaze than when convergence is relaxed. We conjecture that LR MNs with kv < kc and MR MNs with kv > kc innervate muscle fibers that are weak, have mechanical coupling that attenuates their oculorotary force, or serve some nonoculorotary function.
-
Miller JM, Davison RC, Gamlin PD (2011). Motor nucleus activity fails to predict extraocular muscle forces in ocular convergence. Journal of Neurophysiology, vol 105, pgs 2863-2873. (Paper PDF).
|
|
Critiques
Can the once-vigorous field of oculomotor physiology distinguish science from pseudo-science?
|
|
Almost a decade of work from the Demer lab at the Jules Stein Eye Institute of UCLA, reported in over 100 publications and supported by more than $5M in public funds, is shown to be so broadly and deeply defective as to have no value, scientific or otherwise. The Demer lab responds to this critique with a retorical trick, without addressing any of the many substantive issues. This highlights a protracted failure of peer review and of major journals as gatekeepers.
-
Miller JM (2018). Re: Clark RA, Demer JL (2018b). Magnetic Resonance Imaging of the Globe-Tendon Interface for Extraocular Muscles: Is there an “Arc of Contact”? American Journal of Ophthalmology, doi: 10.1016/j.ajo.2018.07.002. (PDF).
The experimental manipulation is inappropriate, the MRI analysis fallacious, and the effect sizes claimed are minuscule in this hoax-like embarrassment of journal peer review.
-
Miller JM, Scott AB (2018). Re: Clark RA, Demer JL (2018a). The Globe’s Eccentric Rotational Axis: Why Medial Rectus Surgery Is More Potent than Lateral Rectus Surgery. Ophthalmology ;125:1234-8 (PDF).
[1] The raison d'être of this study is a misrepresentation of existing biomechanical strabismus models. [2] Their “eccentric axis” hypothesis is based on misleading biomechanics that likens eye muscles to bicycle chains. [3] Their methodology is nonsensical, yielding results unrelated to center of rotation. [4] Their MRI measurements are obviously inaccurate. [5] Their Discussion is innumerate. Ophthalmology retracted the paper when the authors made the tactical error of trying to swap-in a "corrected" methodology after publication.
|
|
Did Jacques René Tenon discover M-D Pulleys in 1805?
|
|
The purpose of the 2019 IOVS paper, “EOM Pulleys and Sequelae: A Critical Review” (Paper & Letters, PDF;Publisher's site; see above), was to distinguish the unexpected functions of orbital tissues described by Miller, Demer and others (“M-D Pulleys”) from disproven and conjectural notions that followed, not to award credit, and not to review 19th century history. COPE, ARVO, and IOVS have all rejected Simonsz’ allegations, and I (Miller) should say something as well.
Haupt Simonsz of Erasmus Medical Center in Rotterdam charged that by assigning the “discovery of EOM pulleys” to a period around 1990 I wrongfully claimed scientific priority, thereby committing scientific misconduct. Perhaps I should have written “modern EOM pulleys”, but in any case it was clearly understood that the point was not anatomic (eg, smooth muscle, connective tissues and encapsulated orbital fat all seemed involved to unknown degrees), but functional. Pulleys solved a problem long assumed to require the brain, but for which no brain center could be found, ie, how was it possible for separate horizontal and vertical gaze centers to control Listings Law eye rotation? Accordingly, I credited the discovery to the Demer, Optican, Raphan, Dean, and Angelaki labs, as well as my own. Around the time I was a Fellow in Dave Robinson’s lab I indeed had a related discussion with Simonsz, but collegial conversations are often not cited in published work.
Simonsz' complaints of neglect reach back two centuries to Tenon, who in 1805 referred to tissues connecting LR and orbit as "poulies”, leading him to claim he was the true discoverer. But Listing wasn’t born until 3 years later so this couldn’t have been about his kinematics. Nor did it involve the modeling, imaging or alert primate studies that form the modern EOM pulley concept. Tenon’s nomenclature is an amusing coincidence, but not a reference to M-D Pulleys.
|
|
Presentations
|
-
Cunha TM, Miller JM, Scott AB (2018).
Injection of Bupivacaine and Botulinum Type A Toxin to Treat Strabismus.
AAPOS Meeting.
(PDF)
-
Cunha TM, Miller JM, Scott AB (2018).
Injections to Treat Strabismus.
Jampolsky Fellows Meeting.
(PDF)
-
Miller JM (2017).
SRF Board of Directors Meeting, 2017.07.13.
SRF.
(Keynote, Powerpoint, PDF)
-
Akhtar N (2017).
Insulin-like Growth Factor-1 (IGF-1) and muscle hypertrophy.
SRF
(PDF)
-
Miller JM (2017).
Explanatory & pragmatic research.
Eidactics.
(PDF)
-
Miller JM (2017).
Non-inferiority testing.
Eidactics.
(PDF)
-
Miller JM (2016).
The Orbit™ Gaze Mechanics Simulation.
Eidactics.
(PDF)
-
Miller JM, Debert I (2016).
History of Botulinum Toxin Therapy.
SRF
(PDF)
-
Miller JM, Scott AB, Debert I (2016).
Bupivacaine Injection Treatment of Strabismus.
SRF
(PDF)
|
|
FabLab
Devices developed for our work that may be useful for yours.
|

|
Extraocular Muscle Force Transducers (MFTs)
The only way to measure physiological oculorotational eye muscle forces.
|
|
|
|
Eye Stabilization Devices
Many clinical and experimental procedures require that the eye of an alert subject be held steady. This is conventionally done with special forceps or suction devices (and topical anesthesia), but neither is safe and effective for more than a few minutes. We're developing two devices: [1] A corneal suction ring that prevents globe deformation and the increase in intraocular pressure that limits application time of existing suction devices. Fabrication is by stereolithography, which makes it possible to customize size and shape for individual eyes. [2] An implantable magnetic detent, also customizable.
|
|
MethLab
Unique methodologies for oculomotor research
|
|
Orbit™ 1.8.3 (OOI 64 bit)
Run Orbit under OSX on your Intel Mac! The Orbit 1.8 Gaze Mechanics Simulation remains the most powerful, reliable, and informative simulation of ocular static mechanics and strabismus.
Orbit 1.8 is a unique research and educational tool that provides a sophisticated biomechanical model able to simulate classical strabismus syndromes and data from individual cases, clarifying diagnostic and treatment possibilities in well-defined physiologic terms. It is is used all over the world by Ophthalmologists, Optometrists, and Orthoptists to model complex cyclo-vertical and innervational disorders and refine their diagnostic and treatment-planning skills, by researchers in vision and oculomotility to study orbital mechanics (eg, to distinguish orbital from central factors), by teachers to supplement the ophthalmology curriculum with strabismus simulation laboratories, and by students to consolidate loosely connected facts and observations into a solid sense of how the extraocular muscles work.
Orbit analyzes extraocular mechanical (eg, globe dimensions, contractile forces, and muscle insertions, lengths, and stiffnesses) and innervational factors in eye alignment. It contains model eyes one uses to test suspected causes of motility disorders and proposed treatments, and a simulated eye alignment test, which shows how the model eyes behave, for comparison with clinical data or desired treatment outcomes. Orbit is related to the ophthalmotropes of Ruete (1845), Wundt (1862), and others, its main advantage being that its behavior is constrained only by knowledge of orbital mechanics, and not by the materials and mechanisms feasible in a physical model. Orbit solves for forces, innervations, and other parameters, according to equations given by Robinson (1975) and Miller and Robinson (1984).
Orbit 1.8.3 has the emulation environment updates required for OSX 10.5 Catalina.
|
|
|
|
Extraocular Muscle Scan Analysis
Since we introduced measurement of EOMs in alert humans using MRI (Miller, 1989), our methods have been used (and misused) to conduct scientific and clinical studies of muscle size, path, and contractile state. Improved methods are now available for quantifying crossectional areas and volumes, and for minimizing measurement errors and biases.
|
|
|
|
Segmenting & Quantifying Muscle Fibers in Stained EOM Crossections
Quantitative histology of extraocular muscles (EOMs) has required sampling because of the many thousands of fibers in a crossectional slice, but unfortunately EOM is highly inhomogeneous making it difficult or impossible to avoid bias. We’ve developed an operator-aided automatic process to segment essentially all the fibers in a section, calculating fiber areas and other statistics, while excluding voids, connective tissues, blood vessels, and nerves. Exhaustive measurement is achieved with only the labor normally required for sampling.
A watershed algorithm segments the histological image, and filters then select the segments with shapes and colors of muscle fibers. Omitted fibers are added, grouped fibers are split, and fiber fragments are merged manually, with computer-aided tools (IPP-9.1).
Early results suggest that BPX injection changes the distribution of muscle fiber diameters in favor of larger fibers, clarifying the nature of the muscle size changes and alignment corrections observed in the clinic. Time-course studies may tell if selective destruction or biased rebuilding is responsible.
|
|
|
|
EOM Fiber Segmentation. Fibers outlined in yellow were automatically segmented (~80%); those in other colors required manual intervention.
|
Effect of BPX Injection On Muscle Fiber Size. Crossectional areas of all fibers in posterior sections (6 mm anterior to the muscle origin) of rabbit SR muscles 30 days after injection with
BPX or saline.
|
|
|
Former Facilities
|

In Jan 2013 I (Miller) left the troubled Smith-Kettlewell Eye Research Institute, and moved my lab to San Francisco's landmark Medical Arts Building. Alan soon joined me. Our facilities were configured for immunohistochemistry, micro-device development, CAD and image analysis.
We conducted clinical studies at California Pacific Medical Center under supervision of their IRB, and physiological studies at several Bay Area CROs under supervision of their IACUCs.
We closed the lab at the end of 2021, and transferred much of the specialized equipment to UCSD, where it will be utilized in related research.
|
|



