|
Our initial intent was to determine the innervation-length-tension relationships of extraocular muscles (EOMs) under physiologic conditions (that is, with normally related innervation and length changes), in order to contribute hard data to the ongoing development of biomechanical models of ocular statics and strabismus.

|
Robinson DA (1975).
A quantitative analysis of extraocular muscle cooperation and squint. Investigative Ophthalmology & Visual Science, vol 14, isu 11, pgs 801-25.
|
 |
Clement RA (1982). Computer simulation of extraocular muscle cooperation: An evaluation. Ophthalmology and Physiological Optics, vol 2, pgs 107-117. |
 |
Miller JM, Robinson DA (1984). A model of the mechanics of binocular alignment. Comput Biomed Res, vol 17, isu 5, pgs 436-70. |
 |
Clement RA (1985). A comparison of different models of extraocular muscle cooperation. Ophthalmology and Physiological Optics, vol 5, pgs 165-170. |
 |
Miller JM (1989). Functional anatomy of normal human rectus muscles. Vision Res, vol 29, isu 2, pgs 223-40.
The modern concept of EOM pulleys is first proposed: extraocular muscle sheaths function as pulleys fixed to the orbital wall, significantly affect muscle actions, and require quite different eye movement control signals than muscles without pulleys. The type of no-pulley model that would give rise to "bridle forces" is shown to be wrong. A test of the pulley model is described using MRI data before and after muscle transposition surgery, and early results from such studies are cited to support the pulley model (see Miller et al 1993 for more). |
 |
Simonsz HJ (1990). The mechanics of squint surgery. Paris: CERES. |
 |
Miller JM, Demer JL, Rosenbaum AL (1993). Effect of transposition surgery on rectus muscle paths by magnetic resonance imaging. Ophthalmology, vol 100, isu 4, pgs 475-487.
We report the first test of the pulley model, in which the experiment outlined by Miller (1989) was performed in 4 human strabismus patients. Images of muscle paths, before and after vertical recti were reinserted at the margins of the lateral rectus, showed that the vertical rectus muscle bellies remained close to their pre-operative positions, supporting the pulley model, and leading to subsequent studies of pulley tissue anatomy, histology, and innervation. |
|
Miller JM, Shamaeva I, Pavlovski DS (1995). Orbit 1.8™ gaze mechanics simulation. Eidactics; Suite 404; Greenwich Street; San Francisco, CA 94109; USA. |
Muscle Force Transducer (MFT) for Humans
This MFT can be installed temporarily during eye muscle surgery under local anesthesia.
|
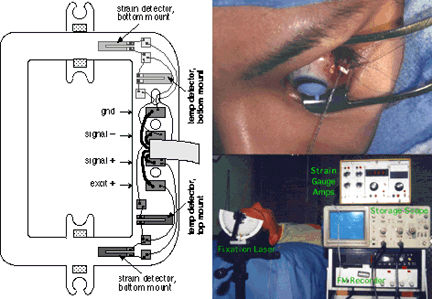
Left Panel: The human MFT contains a full Wheatstone Bridge, 4 strain gauges arranged so that output is compensated for temperature even if the device's top surface (exposed to air) and bottom surface (resting on sclera) are at different temperatures.
Right Panel: Human data collection set-up. The MFT is installed before the muscle is disinserted, with leads projecting forwards. Above the patient's head a laser pointer attached to a position encoder projects a fixation target on the operating room ceiling and records its angular position. A cart holds (a) strain gauge amplifiers, (b) a digital storage scope for viewing muscle force data as it is collected, and (c) an FM tape recorder, for making a permanent record of fixation laser angle, voice annotations, and MFT signals.
|
Digit Flexor Tendon Force
As a spin-off of our EOM force studies we designed a muscle force transducer for the flexor digitorum superficialis tendon of the human middle finger.
|
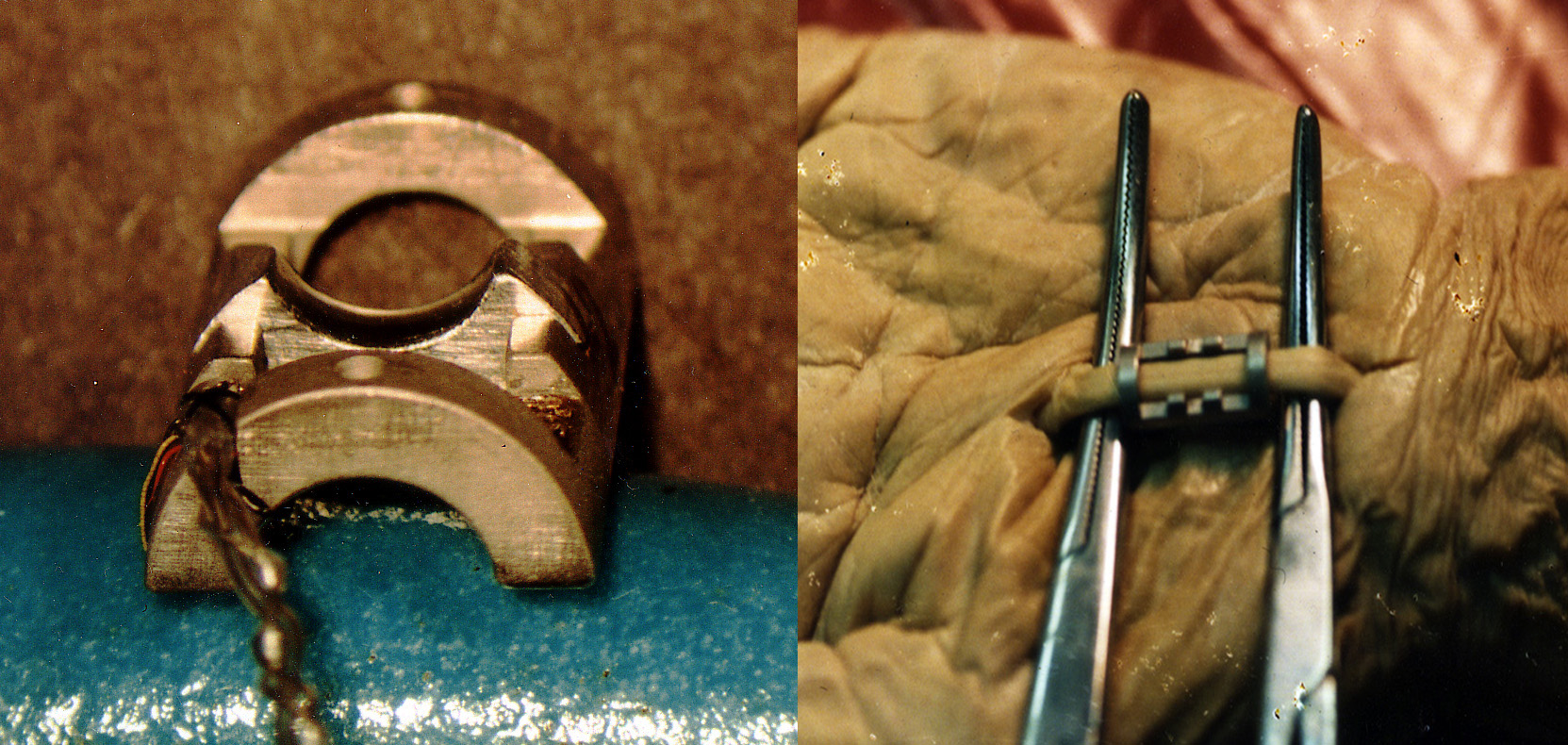
This device was designed to measure much higher forces than the EOM device, and to compactly enclose a tendon having a round crossection. It has been used to study tendon forces associated with key pressing in volunteers undergoing carpal tunnel release surgery.
The Digit Flexor Tendon Force Transducer is a two-part device, shown assembled on the left. The saddle-shaped piece in the middle snaps out for installation, as shown on the right on a cadaveric tendon. When the saddle is replaced under the tendon, the tendon is deflected, so that its tension deforms the transducer frame. A pair of silicon strain gauges is mounted on the top, and another pair on the bottom of the frame. One gauge of each pair measures strain, providing a push-pull signal that sums force aross the tendon, and the other measures temperature, providing compensation separately for the bottom of the device, which is in contact with warm body tissues, and the top, which is in contact with room air. |
Physiological EOM Forces in Alert NHP
We developed first and only way to chronically measure eye muscle forces in an alert behaving animal. Experiments with this device disproved the clinical notion that horizontal EOMs co-contract in convergence, and the "final common path" assumption in oculomotor physiology.
|
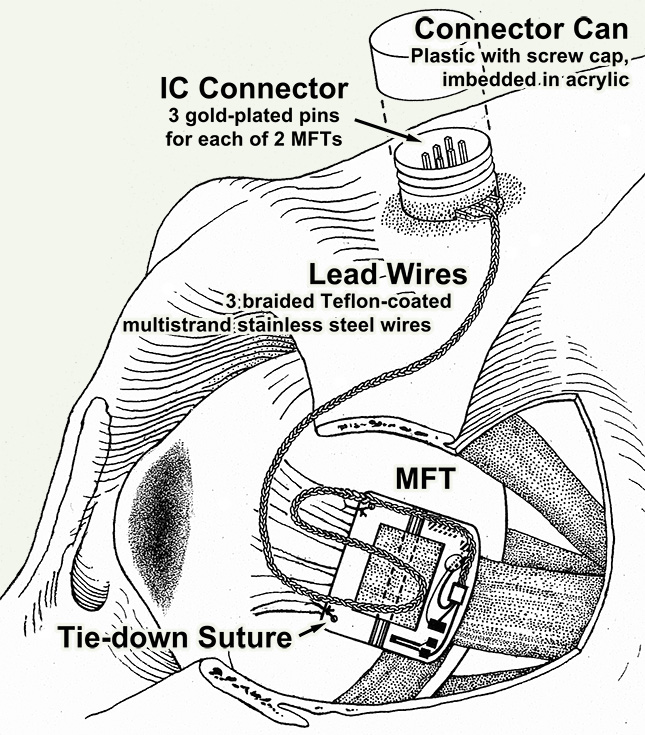
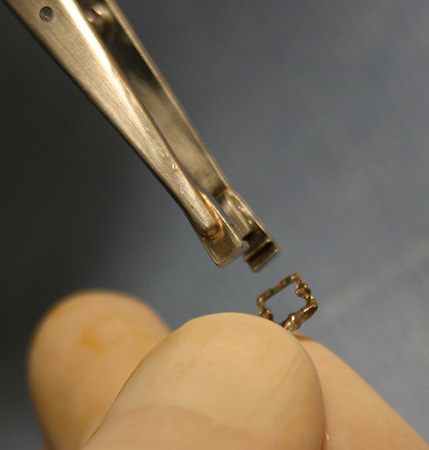
Extraocular Muscle Force Transducers (MFTs) have been implanted on lateral and medial rectus muscles. A properly implanted device can deliver signals for many months. Special tools are used to handle and implant these delicate devices.
|
MFT Fabrication & Implantation

|
Miller JM (2013). MFT Fabrication, Testing & Implantation. Eidactics, San Francisco.
Fabrication and testing details are provided mostly for your information because you will probably not want to undertake this highly specialized, very fussy work. We may be able to fabricate devices for interested investigators, and would be more than happy to receive your suggestions for device and fabrication improvements.
|
|